Liposuction is one of the most popular cosmetic surgical procedures in the U.S. Plastic surgery practices offer liposuction procedures using a variety of technologies. Radiofrequency-assisted liposuction using the FDA approved BodyTite is a popular option among men and women seeking body contouring in NYC. A new study titled “Second Generation Radiofrequency Body Contouring Device: Safety and Efficacy in 300 Local Anesthesia Liposuction Cases”, reports that the second-generation RFAL device offers greater safety and efficiency compared to the first-generation device. The study was authored by bodySCULPT plastic surgeons Dr. Christopher T. Chia MD and Dr. Spero J. Theodorou, and two other surgeons, Joseph A. Marte, MD and Derek D. Ulvila, MD, was published in Plastic and Reconstructive Surgery – Global Open: September 2020 – Volume 8 – Issue 9.
Radiofrequency-assisted liposuction (RFAL) was introduced in the early 2000s and has undergone significant improvements since then. The second-generation device used in this study is the asymmetric bipolar device that has been available in the U.S. since 2016. Several safety features have been added on over the years. Today, RFAL under local anesthesia is a safe and effective body contouring option with significant soft tissue tightening benefits.
The study reported a single center’s experience with two surgeons using the second-generation RFAL device compared with the first-generation device in terms of safety and efficacy. The first- and second-generation device data were collected from the same, single practice location eight years apart.
In the RFAL device, RF energy is delivered between two electrodes in the handpiece: the external one maintaining contact with the skin and the internal probe located within the subcutaneous fat layer. With differing energy delivery, higher temperature levels can be achieved internally than externally. Energy based modalities such as RFAL combined with suction-assisted lipectomy (SAL) can provide effective body contouring along with optimal skin tightening.
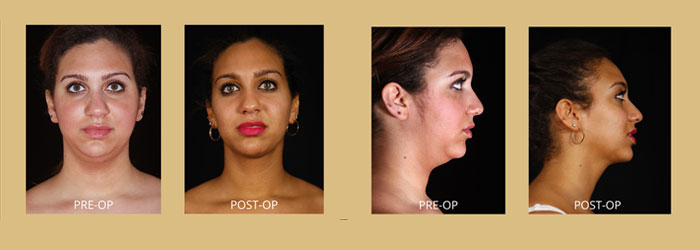
A total of 300 consecutive operations were performed on 240 patients in 421 anatomic areas under local anesthesia, with the patients awake throughout the procedure. Areas treated included the abdomen, arms, axilla, bra roll, breast, cheeks, chest, eyelids, flanks, hip, jowls, and knees. Following tumescent injection, the RFAL device was used to heat the skin and underlying collagen network. Subsequently, excess fat and fluid were removed from areas to be contoured with suction-assisted lipectomy.
The study found that treatment with the second-generation RF device witnessed fewer complications when compared to first-generation RF device. According to the authors, procedures performed using second-generation device had no mortalities, hospitalizations, or major complications compared with the patients who received first generation RFAL treatment.
To compare the second-generation device to the first-generation device, three tests were conducted to find out:
- proportion of major complications
- proportion of minor complications
- proportion of all complications
All three tests indicated that second generation participants demonstrated statistically significant lower proportions of major, minor, or cumulative complications compared with the patients who received first generation RFAL treatment. Major complications were seen for 6.25% of the first-generation group 6.25% and 0% for the second-generation group. The first-generation group showed 8.3% minor complications, while the second-generation group had 0.7%.
“We found that the current iteration of the RFAL device when used judiciously is safe and effective in the group of 300 consecutive cases presented, which were all performed under local anesthesia”, wrote the researchers.
The paper points out that the second-generation device contains several safety features that the first-generation device did not have. Two noteworthy features that improve the safety profile as well as the efficacy of the second generation RFAL device are:
- Internal temperature real-time monitoring with the existing external thermistor
- Temperature surge protection (TSP) which monitors the temperatures internally and externally real-time, and alerts the surgeon if the temperature rises too quickly, avoiding dangerous spikes and preventing burns
The authors also noted that the excellent analgesia achieved would also allow the surgeon to combine RFAL treatment with autologous fat transfer, non-invasive skin treatments and scar revisions with excellent patient compliance and comfort.